A new technique for isolating cells carrying the full fetal genome from cervical swabs could enable doctors to diagnose genetic disorders without using needles to harvest cells from the placenta.
Brown University researchers have developed a simple method for isolating placental cells from cervical swabs. The technique, described in the journal Scientific Reports, could aid in developing less invasive ways of diagnosing genetic disorders in developing fetuses.
The technique isolates trophoblast cells — placental cells that carry the complete fetal genome — by taking advantage of their tendency to settle to the bottom of microwell plates. The researchers lay out a procedure for optimally isolating the cells, enabling them to be picked individually from the plate.
"This is the first study to use cell settling for enriching trophoblast cells from a heterogeneous cervical cell population," the researchers write. "Ultimately, we provide a technique that is quick, inexpensive, minimizes cell loss, and results in retrieval of individual trophoblast cells."
The work was led by the lab of Anubhav Tripathi, a biomedical engineering lab at Brown that specializes in lab-on-a-chip diagnostics — in collaboration with the Shukla Lab for Designer Biomaterials at Brown's School of Engineering, led by Anita Shukla, and with PerkinElmer, Inc.
Currently, the only way to diagnose genetic disorders in developing fetuses is by retrieving trophoblasts through amniocentesis or chorionic villus sampling, both invasive procedures that carry a small risk of miscarriage. Blood tests that look for fetal genetic material in the mother's bloodstream can be useful screening tools, but they can't be used for definitive diagnosis. And screening is limited to whatever genetic material happens to turn up in the blood, which limits the range of disorders that can be screened.
Trophoblasts are known to be present in the cervical canal in the early stages of pregnancy, but the quantities are small, and isolating those cells from cervical cells and mucus is difficult. For this new study, a team of researchers led by Christina Bailey-Hytholt, a Ph.D. candidate in biomedical engineering at Brown, wanted to see if there were any physical characteristics of trophoblasts that might help in isolating them from cervical cells and other material.
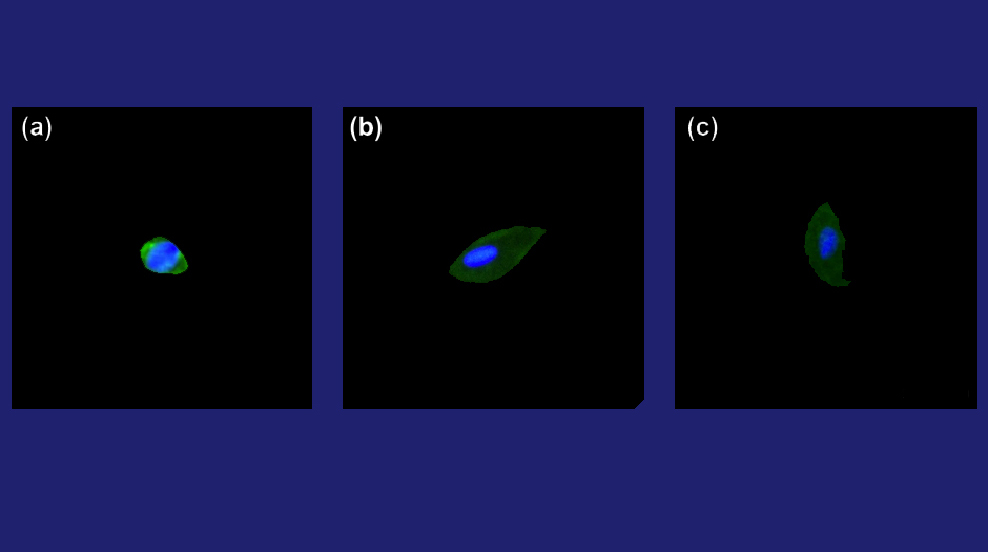
The researchers found that trophoblasts are smaller than cervical cells, differ in shape and have relatively large nuclei. Those characteristics suggested that they may settle more quickly than cervical cells when cell mixtures are placed on microwell plates.
Using polystyrene plates, the researchers found that the trophoblasts did indeed settle more quickly than cervical cells. The study showed that the maximum separation of cell types was achieved around four minutes after the cells were put on the plate. At that point, the cervical cells and mucus on top of the cells could be removed, leaving a large concentration of trophoblasts behind. The technique increased the proportion of trophoblasts in samples by 700%, enabling individual trophoblasts to be picked out for genetic testing.
No specialized equipment beyond what any diagnostic lab would already have is required to perform the technique, the researchers say. And takes only a few minutes to produce the cells necessary for genetic testing.
"There is a large need for biomedical engineering techniques toward advancing prenatal and women's health," Bailey-Hytholt said. "Our work is a step toward more non-invasive prenatal testing options."
Other co-authors on the paper were Sumaiya Sayeed from Brown University, and Morey Kraus and Richard Joseph from PerkinElmer, Inc. The work was supported by PerkinElmer, Inc. and a National Science Foundation graduate research fellowship to Bailey-Hytholt (1644760).