It is estimated that an American suffers a heart attack every 40 seconds. In most cases, the myocardial infarction is caused by a clot blocking blood flow to the heart, and without blood, the heart muscle tissue loses oxygen and dies. Researchers in Associate Professor Kareen Coulombe’s lab are engineering cardiac muscle tissue to regenerate the heart tissue of heart attack survivors.
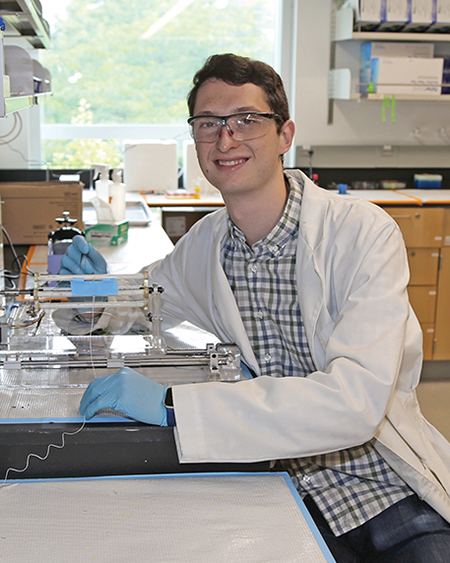 Using the funds from the Neal B. Mitchell ’58 Systems Thinking Project, senior Phillip Schmitt spent the summer developing a tissue scaffold from polycaprolactone (PCL), a biodegradable polymer, with customized fiber architecture. Schmitt’s project involves building a programmable device to automatically collect the fibers into a mesh scaffold and seeding cardiomyocytes onto prepared scaffolds for assessment. He investigates how fiber angle and diameter alter the passive and active mechanical properties of the resulting tissue to assess how scaffold architecture impacts cardiac tissue contractility.
Using the funds from the Neal B. Mitchell ’58 Systems Thinking Project, senior Phillip Schmitt spent the summer developing a tissue scaffold from polycaprolactone (PCL), a biodegradable polymer, with customized fiber architecture. Schmitt’s project involves building a programmable device to automatically collect the fibers into a mesh scaffold and seeding cardiomyocytes onto prepared scaffolds for assessment. He investigates how fiber angle and diameter alter the passive and active mechanical properties of the resulting tissue to assess how scaffold architecture impacts cardiac tissue contractility.
“We’re trying to make a patch to implant onto the heart. What happens during a myocardial infarction is that you get tissue death due to a lack of blood supply, and that tissue doesn’t regrow, so you’re left with scar tissue in the heart, and that can lead to a lot of problems,” Schmitt explained. “So our approach is to create a patch made of living tissue that could be implanted surgically onto the heart.
“My project is a scaffold to put heart cells on that will then grow into beating tissue. The scaffold helps hold them together, giving them time to grow before implantation. Using the PCL, we overlap thin fibers into a mesh-like material, and then put cells on that to create the tissue. The cool thing about polycaprolactone is that it is biodegradable so after a couple years of implantation, those fibers would degrade and disappear, leaving behind all natural-like tissue incorporated into the heart.”
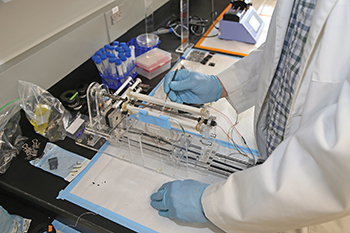
Although others have used PCL for heart applications, the unique part of Schmitt’s project is the technology to precisely position the fibers in a desired orientation and build human cardiac tissue on it. Schmitt spent the better part of the spring semester and the summer designing and fabricating a process for wet-spinning PCL into these aligned fibrous meshes, allowing for a more fine-tuned mimicry of the native heart wall — so that when the heart muscle contracts, the engineered cardiac muscle tissue performs its coordinated contractions that pushes blood flow through the circulatory system. Coulombe says the research will give important insight for anisotropy in future cardiac tissue design and will serve as a stepping stone for additional studies incorporating PCL into therapeutics designed to re-engineer contractility in the injured heart.
As a biomedical engineering concentrator who belongs to Brown’s PLME (Program in Liberal Medicine Education) program, Schmitt gravitated toward this project after taking Biomaterials (ENGN 1490) with Coulombe in the fall of 2019. “I was really intrigued by the work that her lab did and she was very accepting of me,” he said. “I didn’t have much to offer at that point because I was a sophomore and hadn’t taken very many classes in biomedical engineering, but she brought me into the lab and let me see the different projects.
“Right before COVID-19, we narrowed down what I was interested in, and started this project based on previous work by (engineering Ph.D. graduate) Nick Kaiser. He designed a similar scaffold using collagen fibers, so my project was to use a synthetic polymer that can biodegrade rather than a natural polymer like collagen.
“Depending on the results of our data, hopefully it’s something that the lab will continue working on,” he said. “(Doctoral student) Kiera Dwyer is interested in the mechanics of the heart and she’s continuing much of Nick’s work with the collagen fibers. She’s been such a great mentor to me, and, if this goes well, she may use PCL in composite scaffolds.”
Along with a stipend to keep Schmitt on campus last summer, the Mitchell funds also assisted in sending him to the 2021 Biomedical Engineering Society annual meeting in October, where he presented his findings in a research poster. He is hopeful that more data collection will lead to an eventual publication, but for now the project will serve as a basis for his senior thesis.
“I knew I liked the mechanical side of it (from the beginning), and wanted to have something to build, so I thought it would be interesting to do something new like this. Building and creating has always been a hobby of mine,” said the Hamden, Conn. native who has served as Head Mentor for ENGN 30 (Introduction to Engineering) first-year students in the Brown Design Workshop this year. Schmitt is no stranger to the BDW, serving as a monitor and ENGN 30 mentor since his sophomore year.
As a PLME student granted the opportunity to combine undergraduate education and professional studies in medicine into an eight-year program, he is not completely sure where medical school will take him in the future, but “definitely something hands-on, or something with procedures. It might be surgery, or something else.” For Schmitt, that has been at the heart of his plan all along. “It’s mostly me trying to merge my interest in medicine with my interest in engineering. So I think it has all fit together pretty well,” he said.